An Electrician For the Heart On Delivering Personalized Healthcare via 4D Imaging & Artificial Intelligence
/Women Leading Visual Tech: Interview with Dr. Elaine Wan
LDV Capital invests in people building businesses powered by visual technologies. We thrive on collaborating with deep tech teams leveraging computer vision, machine learning, and artificial intelligence to analyze visual data. We are the only venture capital firm with this thesis. We regularly host Vision events – check out when the next one is scheduled.
Our Women Leading Visual Tech series is here to showcase the leading women whose work in visual tech is reshaping business and society.
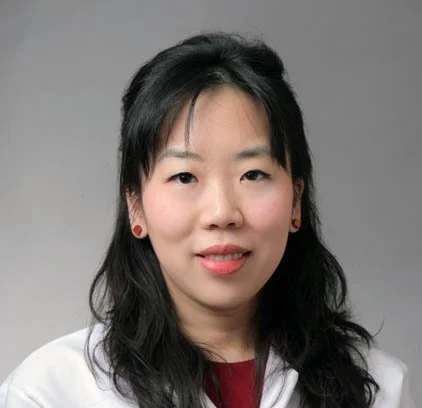
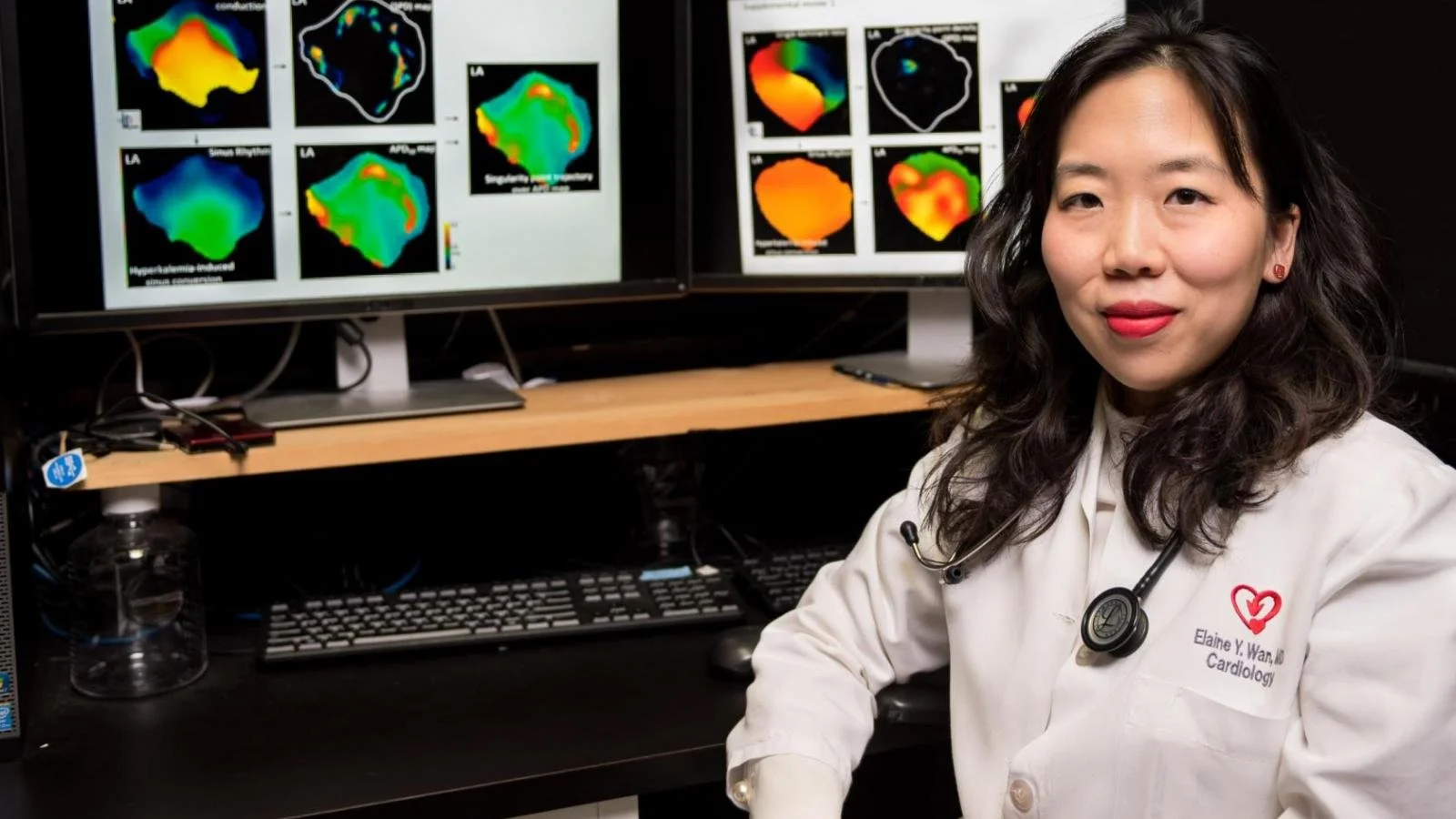
Dr. Elaine Wan is the Esther Aboodi Associate Professor of Medicine in Cardiology and Cardiac Electrophysiology at Columbia University Medical Center, College of Physicians and Surgeons and attending physician at New York-Presbyterian Hospital. At Wan Lab, her research is focused on the vascular and electrophysiological changes that occur in heart failure and atrial fibrillation.
She is trained in internal medicine, clinical cardiology and is an invasive cardiac electrophysiologist. She is the Director of Electrophysiology Research and oversees all electrophysiology clinical trials.
Dr. Wan is a physician-scientist and focuses on the development of novel treatments for heart failure, vascular dysfunction and arrhythmias such as atrial fibrillation. She is a translational researcher also interested in the development of innovative imaging modalities to improve ablation delivery. Dr. Wan is a graduate of the Massachusetts Institute of Technology. She received her medical degree from Columbia University College of Physicians and Surgeons and completed her fellowship in Cardiovascular Diseases and Clinical Cardiac Electrophysiology at New York-Presbyterian/Columbia.
Dr. Wan is the recipient of numerous national and international awards including the 2016 American College of Cardiology Young Investigator Award First Place in Molecular Cellular Cardiology, 2016 Young Physician Investigator Award from the American Society of Clinical Investigators, 2016 Cardiostim/Europace Best Young EP Presentation (Nice, France) and the 2008 American Heart Association Women in Cardiology for Clinical Excellence.
Abigail Hunter-Syed chatted with Elaine about noninvasive 3D imaging of the heart, how AI can help us make sense of all the data that our wearables collect, the impact of COVID-19 on hearts and so much more! (Note: After five years with LDV Capital, Abby decided to leave LDV to take a corporate role with fewer responsibilities that will allow her to have more time to focus on her young kids during these crazy times.)
The following is the shortened text version of the interview and the unedited video can be found below.
Abby: How would you describe what you do to a 2-year-old?
Elaine: If you think of the heart as a house, a house has many parts. There's electrical and there's plumbing. If there's a problem with the pipes or clog, then you have a plumber – an interventional cardiologist who opens up the clog to fix the pipe. If there's something wrong with the electricity of the house, you call an electrician and that's exactly what I am. I'm an electrician for the heart.
How do you fix the electricity? Well, either there's a short in the system, so you fix the short in the electrical circuit, or sometimes the wiring is broken, then you need to put in a new wire to have a new way to connect the electrical system. I do both of those things.
Abby: Did you always want to be a doctor? What was it about medicine that drew you in?
Elaine: I was always fascinated by science. In my younger years, I wanted to be like a cardiothoracic surgeon, like Dr. Memenaz or Ben Carson. Growing up, I was reading their stories about how they use their hands to fix things. There's something gratifying about using your hands to directly fix someone or something.
I quickly realized that the field of cardiology and medicine was moving towards more minimally invasive methods, like using catheters and wires to reach the heart to fix things. I pursued a career in interventional cardiology specifically for the electricity of the heart and I'm glad that I did because that's definitely where we are currently and continuing to grow.
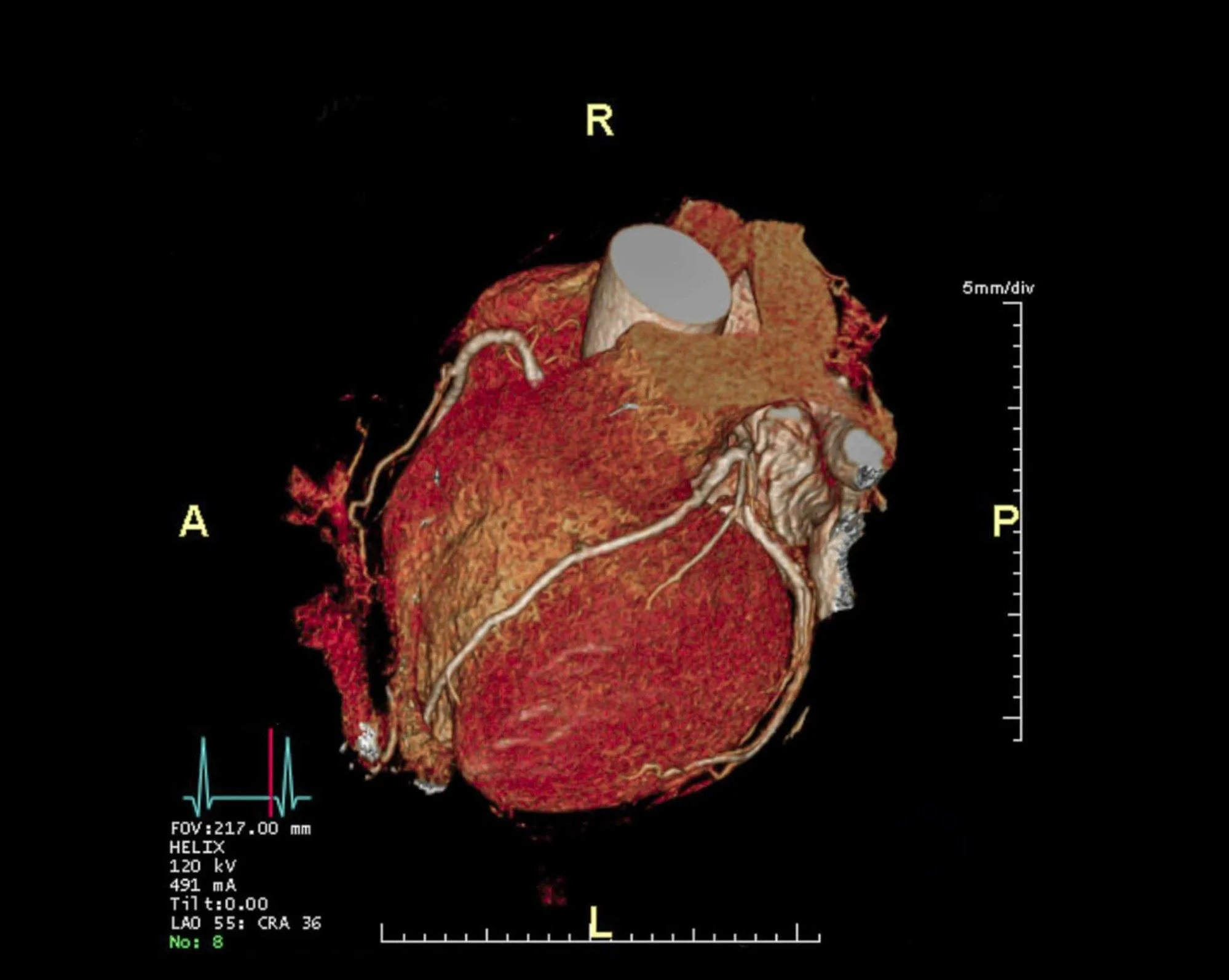
Heart CT scan © Echelon Health
Abby: When did you start leveraging imaging modalities and deep tech, like machine learning and computer vision, to provide more personalized therapy or care for patients with heart issues?
Elaine: In medical school, we learn about how patients are different. Obviously, the physiology of men and women is different. Racial differences also come to play. We can't treat everyone's heart the same way. We have to look at the heart itself.
One way to do that is through imaging. We're all familiar with chest x-rays. We also look at the electrical signal of the heart, an EKG.
There are different ways to look at imaging the structure of the heart. You can use ultrasound, CAT scan, or MRI.
The heart is a 3D object, so there are many, many curvatures. When you look at only a 2D slice of it, you're missing a lot of information about the curvature of the heart.
The structural abnormality is like the thickness of the tissue, the size of the organ itself. We need to personalize our treatment for our patients by using imaging to look at the biological process within each patient and also help stratify them to figure out individual treatments for these patients. Lastly, we need to follow the progress of their treatment, to see how they're doing over time, and whether or not they're responsive to the treatment or not. The inspiration behind this is to deliver personalized treatment to each patient.
Abby: Why do you think it's only now that CAT scans and MRIs are finally being used to get a 3D picture of the heart?
Elaine: It's thanks to all those advances in technology.
A chest x-ray is just a 2D image of a 3D body. When you look at an x-ray, it’s just black and white. Now, we're looking at different colors, different structures, and different cross-sections with higher resolution.
It's hard to combine all that data. That's why all these new modalities like machine learning and deep neural network learning are used to put that all together. Advances in technology to synthesize the data and also to capture the data have allowed us to propel all of the science even further.
Abby: You mentioned thickness, for example. Is that something that could never be known before with the existing types of heart diagnostics that were out there? Could you give me an example of how something that's picked up on a 3D image impacts diagnosis and treatment?
Elaine: In the world of interventional cardiology, there're so many new ways of imaging. Now we don't even think of 3D, but we think of 4D, and what 4D is, is looking at a velocity over time. A 3D image is an image at one time and as you know, the heart is an organ that keeps on pumping, filling, and contracting over time, and we want to see the movement of the heart over time. So now there's even 4D imaging. There are a lot of advances in that.
Valves are one of the examples where 3D and 4D imaging is currently used. If you think of a valve as sort of like a valve and a pipe, if the valve is weak, you want to see how much it leaks over time through a contraction and relaxation of the heart. In 3D, you can see where the leakage is. In 4D over time, you can see what is the velocity of the leakage and what area. You can also see the thickness of the tissue. When you do a cross-section through the heart, where are the thin areas? Where are the thick areas? For example, athletes might develop a thickened heart wall because they've been excessively exercising.
We want to measure the thickness of the heart tissue over time. That can be done using 3D reconstruction of images or even cross-sectional images of the heart. These are important things that we're now looking into and will continue to look into different velocities and time and thickness, and tissue structure.
Abby: That's fascinating that even 3D and 4D are pushing the envelope in terms of non-invasive ways to view inside the body and specifically the heart. I saw that you've done a bunch of work on taking 2D video and analyzing it via deep learning to get some of the same insights that you might be able to through other scanning mechanisms. Do you believe that we need to have so many different new types of modalities to look at it or do you think that algorithmically you can solve for given what the current monitoring mechanisms are today?
Elaine: Having more dimensions adds more data and value for our patients because when you're talking about the heart, you want to be as precise as possible. You want to know the sizing of a valve, or when we put like a wire, like a pacemaker through the heart, we want to be accurate where it's going or when we're doing inflation of the heart. We only want to burn the tissue which is short and the electrical system to treat the area that's causing the problem.
It’s important for us to be as precise as possible. If you think of the heart, it's the size of your fist. It's not too big. You don't want to be a bull in a China shop and burn or treat all the areas. You treat areas that need to be treated. Having more refined imaging is helpful.
Abby: Precision sounds great to me as a patient. 10 years from now a patient who's at risk of heart failure, what kind of devices or techniques do you think doctors are going to be using to monitor them remotely?
Elaine: Digital health has been propelled forward by the COVID 19 pandemic. Now with all the technology, it's convenient to use your Apple Watch, Fitbit, or your smartphone to send an array of data to your physicians about your heart rate, your electrocardiogram, and how many hours of activity you've exercised, etc. A lot of new devices, wearables, have been marketed to consumers to help them check what's going on.
It's gone beyond just like a scale in your weight. Wearables can either be put on your skin or implanted. There are loop recorders that go underneath the skin and constantly track data. They have huge battery life and can give real-time data to your physicians. You can also record data for yourself about whether or not you have any heart arrhythmias.
The technology can tell you information about how many hours you slept, what your heart rate variability was, the angle in which you slept, how many pillows you used, etc. because you were short of breath and that you might be at risk for a heart failure episode. A lot of data is coming out of all these wearables.
Consumers have so many choices and the key is there's such a data deluge. What do we do with all this data? My patients will either email me or message me either their EKGs or what their watch says and it's hard to keep up with all of that.
It would be great to have this data put into some sort of electronic medical record that can be shared with all your doctors. It's not uncommon for patients to have four to five doctors if they have multiple medical problems. Lastly, it would be great to have some sort of machine learning algorithm to flag important things.
It would be important for me to know about atrial fibrillation because the patient would be at risk for stroke, but if it's just an extra beat or skips a beat, that's common in a benign arrhythmia, it can be a benign arrhythmia.
It'd be important to know which patients I should prioritize. I'd take more time to explain to them what's going on. I’m excited about the future and looking forward to new technology to help physicians and patients work together with all of this digital health data.
Abby: Hopefully five years down the road, there'll be ways of taking this data and leveraging it as you look at the images to not only see what's going on but then to have an understanding of how it's gotten to that point or how it's improved or worsened over time, given all of the data from in between that you've gathered about the way that the patient's living their life. Some of your recent research is focused on the impact of COVID-19 on hearts. What is the biggest takeaway from your research so far that people should know?
Elaine: We were the epicenter when we had the first wave in New York City and it was a big shock to us at that time not knowing what to expect. Even right now, a lot of us had the post-traumatic stress of seeing patients who were young and old who got so sick so quickly. At that time when we were shut down and taking turns, working on the ward service, we did all our best to try to learn about the disease.
That's our way of trying to be proactive to help. I have two articles that were published in Nature Medicine. One was about the acute effects of what we saw then, multi organs, the systemic disorder of COVID 19. The other article was about long COVID, about the remaining, the post-acute long-lasting effects that we saw.
COVID was causing both plumbing and electrical issues. We had patients that had acute clot development in their blood vessels that caused a heart attack, and then we saw patients who suddenly either had heart block, which means the conduction system was not working and they needed a pacemaker, or they suddenly went into cardiac arrest because they had a short in their electrical system and they went into the dangerous arrhythmia of ventricular tachycardia, ventricular fibrillation.
We saw a wide array of different arrhythmias. The most common was atrial fibrillation. On normal days, atrial fibrillation is a common arrhythmia, but when patients had full-on systemic inflammation and had other comorbidities brought about by COVID, we saw more and more patients with atrial fibrillation and we showed in one of our articles that if you had COVID and you had atrial fibrillation with some sort of mild cardio injury, you were at a higher risk of having complication in the hospital and a higher risk of death with COVID. The great news is that thanks to the advance in science, we had the RNA vaccinations available, and now the most recent Omicron surge, most people only had a mild case.
We didn't see any of the mild cardiac inflammation and disastrous deleterious effects of COVID that we saw in the first wave, but it was important for us to document it because we were one of the first cities to see that and that we could share with our colleagues to look, to be aware and cautious that this is what they might see in their patients as the virus spread throughout the nation. That was the motivation behind all of that.
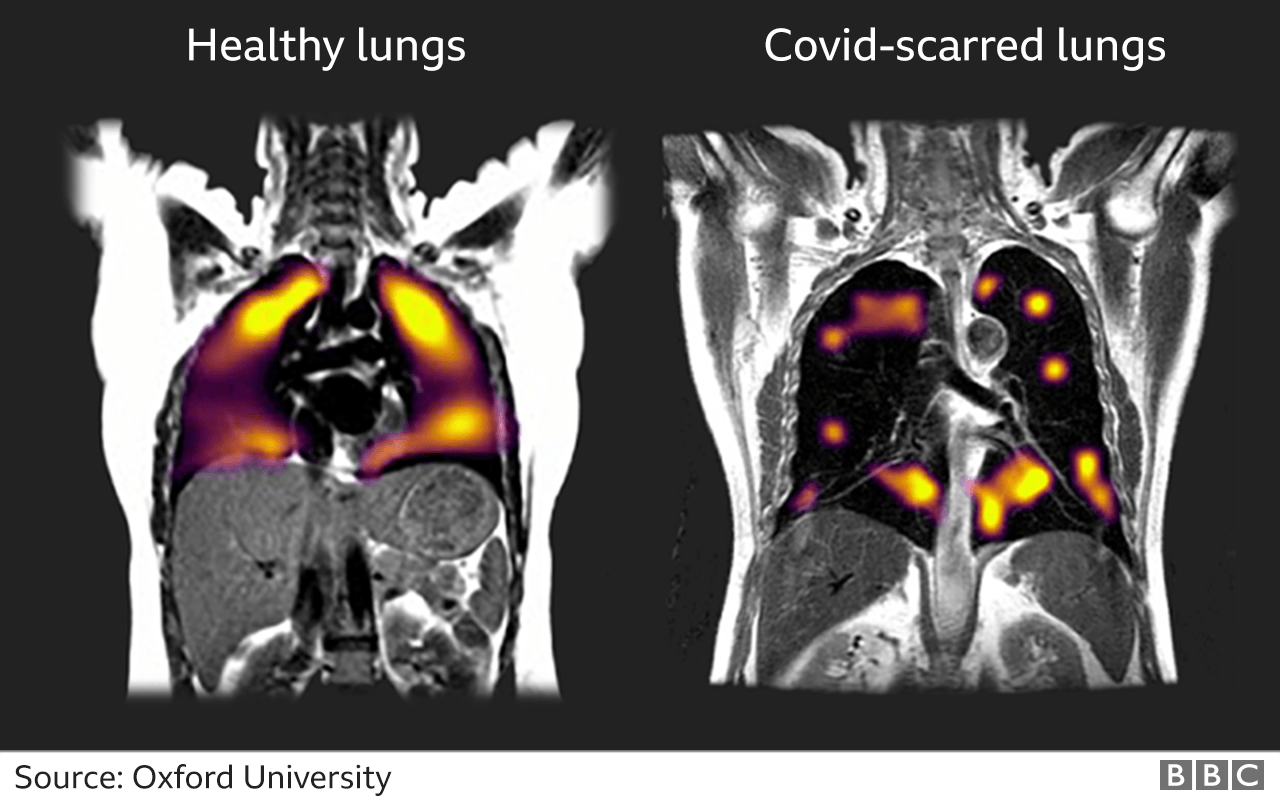
Abby: It's such great news that we're seeing much less of the high-risk cases today! I saw a recent paper, where a few images of lungs impacted by COVID were showcased. Are there pictures of the heart showcasing a COVID impact?
Elaine: Remember we talked about the chest x-ray? There's radiation involved, unfortunately, but it's just like a black and white picture and it's easy to do. The cost is very low. For imaging of the heart, there are difficulties in that, for example, an MRI which can be built together to give information about the heart in three dimensions is time-consuming and costly.
The key is to personalize imaging of the heart so we can personalize treatment for patients.
Abby: You've also done some work into looking at the disparities of our healthcare system, particularly on the misclassification of sudden cardiac death and then out-of-hospital sudden death for women and people of color. If I read between the lines, this idea of imaging and getting a better idea to personalize the healthcare of each individual, do you think that that's going to play a major role in overcoming some of these disparities and the failings of the healthcare system because they've been treating everybody the same?
Elaine: It's a complex question because one, there has to be the availability of the technology, and two, most importantly, access to the technology, right?
The COVID pandemic has highlighted that these are ongoing issues that are difficult to answer in a short period, but if there was more access to widely available technology, then hopefully that could allow us to personalize treatment and monitoring of healthcare for different patients. We need to solve more simple problems first like testing and blood tests, etc. before we do even more complex things like complex imaging.
What we had is the understanding of the genetic build-up of each person. Now we know what your genes are, what is being expressed and what's not, and what's going in your body now. Imaging is helpful for that because sometimes you might have the genes but that doesn't mean that it's being expressed or turned on. The question is: what is being turned on? What has some intervention affected what's going on right now? You bring up great examples of chest x-ray or CT scans for the lungs. We want to advance imaging for the heart and specifically for things such as cardiac arrhythmias, because it's a common diagnosis to have atrial fibrillation or people with palpitations feeling skip beats, what is going on with their heart that might cause them to feel this or have this.
Abby: I'm going to change pace just a little here. I’d love to know your perspective on how the cardiology world looks for women who enter it today. What was it like when you entered cardiology? Do you feel it is supportive of women? How do you think it's changed over the past few years?
Elaine: I'm thankful for my colleagues who are supportive. Currently, I'm the only woman faculty in the cardiac electrophysiology field but I'm happy to share that we hired a second woman, which is great. I'm supportive of it and our program is one of the most proactive about recruiting women.
Currently, we have three female fellows as electrophysiologists, and we've graduated at least five or six and they've gone on to become independent women managing their laboratories. Our field at Columbia EP is supportive of women. Overall, when I first started my cardiology fellowship, women were not anywhere near the halfway mark. There were only two of us and the rest of my class were men. But once again, all my male colleagues were supportive. They always treated me as an equal, taking calls or taking care of sick patients, seeing how they could help me if I were on a very, very busy day or had a lot of critically ill patients.
I was lucky to have a supportive environment. There’s now an initiative at Columbia to provide inclusivity and a sense of belonging for all comers, healthcare providers, and students of a different race, gender, or sexual orientation. That's important because that reflects the providers that can provide care to patients and our patients are diverse.
It's only through having these different providers that they could advocate for these patients and advocate for example, that physicians should have diversity and should have an equal mix of women and men and a diversity in who they recruit and who practices it. That's one major way of counteracting all the disparities that we see.
You and I are both women and you interview all the women in science, and there are a lot of things that we don't share or are afraid to share. One for example is the peripartum period, the postpartum period, and then transitioning back to work. Those are difficult times. I can tell you that I'm an academic physician-scientist and this time raising a young family, especially in the setting of the COVID pandemic is the most difficult time I've ever had in my career.
In the peripartum period, if you're lucky, you don't have that many symptoms or you might have hyperemesis gravidarum where you feel constantly sick, which is morning sickness if you have that all the time. In the postpartum period, you have to struggle with, if your infant is sleeping well or not, and breastfeeding and lactation, which is tough for us who were wearing heavy lead all the time. Right?
You're feeling constricted. You don't have time to pump or make sure that your child has the nutrition that you want to provide him or her. Then it's the transition back from maternity leave where you're devoting all your time to your infant, your child, and then it's like an on-off switch where you suddenly just have to go back to work. There's no in-between for some jobs.
Certain jobs where you have to be on-site and you're not working remotely. Before we started this conversation, we chatted about the fact that the COVID pandemic has been hard for daycare. Being in quarantine, all of us have been on some sort of daycare or school quarantine, because any you or I already flagged and children, being sick is what they're all about when they're all together. Then if you're lucky, you don't get sick with them, but if you're sick, everyone's sick and then you still have to do your job. It's another full-time job. We're making advances but there are a lot of other things that can be done to be helpful.
For women in science, the tenure track is a difficult thing to achieve. Maintaining productivity, getting grants and writing papers, and being a mom is a full-time job and you don't want to feel like you’re sacrificing being a mother or wife or a daughter for attaining your career goals. I look forward to women working together to be more proactive to advocate for each other. I'm a big proponent of women supporting each other.
I'm so glad that one of the ways I got to where I was, is having great female mentors. What's a good thing is having women in leadership roles to promote these needs. If you don't have women in a position to advocate for these needs, then the rest of us will never have speaking or a time to talk about what we need to allow us to have success.
Abby: I second everything that you mentioned. One of the big things that we talk about in the venture is how women fund women at much larger proportions than men do, and women help women. Even talking about coming back from maternity leave and trying to find somewhere to pump in between back to back to back patient visits; as supportive as some men are, these are issues they just don't have.
Having an advocate for you at the upper echelons of your university or your practice, or your firm becomes an important part of furthering women in the workforce as a whole.
Hope you enjoyed this interview as much as we did! Check out other interviews in this series on our newly-created YouTube channel.